Case Series
Stuart J. Froum DDS, Sang-Choon Cho DDS, Kibong Kim DDS
Foreword
Fiona M. Collins BDS, MBA, MA
We are pleased to provide this CE course titled “Removal of Failed Integrated Implants Using Minimally Invasive
Techniques,” written by Drs. Stuart J. Froum, Sang-Choon Cho, and Kibong Kim.
This article begins with a discussion on the indications for removal of integrated implants, prior to discussing the
available methodologies for doing so. The authors present options for implant removal with recommendations and
descriptions on the use of the least invasive techniques where possible. This is followed by a review of bone removal
techniques with greater and varying degrees of invasiveness. A case that involved the removal of multiple implants using
both minimally invasive and bone removal techniques is also presented.
As discussed in the article, using a technique that is minimally invasive reduces trauma and preserves the site for
future treatment. The utility of each technique, its limitations and contraindications, and recommendations for implant
removal are addressed.
With the increasingly large number of implants now placed globally every year, implant failures due to peri-implantitis
as well as implant and component failures can and do occur. This article provides timely and practical information on the
removal of failed integrated implants. We hope that you will find this article educational and useful for your practice.
As always, we welcome your feedback on this article and any suggestion you may have for future topics.
Abstract
Failure of osseointegrated implants can occur due to several etiologies, including implant fracture, implant malpositioning and periimplantitis. Techniques available for the removal of failed implants include counter-ratchet techniques; reverse screw techniques; and the use of piezo tips, high-speed burs and trephines for bone removal around implants. The removal of failed, nonmobile implants requires
careful consideration of the least invasive technique that can be used in a given situation as well as the post-removal site.
EDUCATIONAL OBJECTIVES
The overall goal of this article is to provide the reader with information on the frequency of use of the various implant removal
techniques at one clinical teaching center. Information is provided on each of the removal techniques, with emphasis on the indications,
effectiveness, limitations and complications of each technique when removing a hopeless but still integrated implant.
On completing this article, the reader will be able to do the following:
1. List the etiologies of failed implants;
2. Describe the counter-ratchet and reverse screw techniques that can be utilized for minimally invasive implant removal;
3. Review the indications and use of piezo tips and high-speed burs for implant removal;
4. Review the use of trephine burs for implant removal and the technique that should be used; and
5. List and describe the considerations and limitations in selecting an implant removal technique.
Removal of Failed Integrated Implants Using Minimally Invasive Techniques
Introduction
The use of dental implants in the treatment of total or partial edentulism has demonstrated a high degree of success, with documented survival rates of 90% to 97%.
1,2 Although improvements in implant design and surface microtopography in recent years have resulted in increased success rates of dental implants, between 3% and 10% of implants still fail.
3,4 With the approximately 2 million new implants that are placed worldwide every year, and tens of millions of dental implants currently in
function, the estimated number of implants that are failing annually is estimated to be in the range of 200,000–250,000.
5 Meanwhile, criteria to determine successful integration of dental implants have been proposed.
6 Among these, lack of mobility is a primary prerequisite.
In cases where an implant demonstrates mobility, all parts of the implant should be immediately removed to prevent progressive destruction of the surrounding tissue. However, even when implants have no mobility, indications for their removal include implant fracture, alposition, infection, pain and advanced peri-implantitis.
6 In many cases, failed but nonmobile implants are removed by surgical intervention. Various methods of implant removal are available and include the use of a counter-ratchet technique (CRT), reverse screw technique (RST), piezo tips, high-speed burs, elevators, forceps and
trephine burs.
Material and Methods
Clinical data in this study was obtained from the Implant Database (ID), which was certified by the Office of Quality Assurance at the New York University College of Dentistry (NYUCD) Kriser Dental Center.
This data was extracted as de-identified information from the routine treatment of patients at the Ashman Department of Periodontology and Implant Dentistry (ADPID) at the NYUCD.
This use of the database was in compliance with the Health Insurance Portability and Accountability Act (HIPAA) requirements and pproved by the University Committee on Activities Involving Human Subjects.
Advanced peri-implantitis with prolonged pain or signs of continuous infection, fractured implants at either the time of insertion or any time following loading, and malpositioned implants in the esthetic zone with occurrence of peri-implantitis were included in this study.
All of these failed implants showed no mobility, which was assessed on freestanding implants by the application of pressure by two opposing
instruments. If a prosthesis was present, this was evaluated for mobility and an assessment made to determine whether the prosthesis or
the supporting implant (requiring removal of the prosthesis) was mobile. From September 2010 to January 2012,
67 failed, nonmobile dental implants were removed in the ADPID at the NYUCD Kriser Dental Center. At the time of implant removal, a decision tree from a previous article was used to select the least invasive removal technique. Generally, these techniques are used alone or in combination, depending on the clinical situation. However, when removal of an implant is necessary, the least invasive method should be the first option, in order to preserve the site for the possible future treatment and allow for an esthetic replacement, whether an implant restoration or pontic.
7 For cases amenable to removal with the least invasive method, the implant connection, implant diameter, implant geometry, amount of osseointegration remaining, and patency of the internal or external connection were evaluated. Following this evaluation, when the
counter-ratchet technique (CRT) was used to remove the implant, the mount and the torque driver of the corresponding implant manufacturer were utilized.Whenever the reverse screw technique (RST) was used, the conical explant kit (CEK, EBIInc.,Kyungsan, South Korea) was utilized (Fig.1).
The instrument was inserted manually and turned counterclockwise. Torque was applied with a torque wrench (Sybron,Orange,CA) until the
implant was mobilized. Bone removal techniques or combination techniques were used when CRT and RST failed or were not able to be used to retrieve the implants planned for removal.
Results
Of the total of 67 nonmobile implants diagnosed as failed and surgically removed, peri-implantitis affected 36 implants, 8 implants were fractured, 5 maxillary anterior implants were malpositioned and the remaining 18 failed implants presented with a combined etiology. The frequency of use of CRT, RST,BRT (bone removal technique) and combination technique are summarized inTable 1.
The rates of use of each of these techniques were 25.4%, 34.3%, 23.9% and 16.4%, respectively.
Discussion
Approximately 60% of the implants in this case report were removed by minimally invasive techniques (CRT and RST). The RST (CEK) alone was able to remove more than 1⁄3 of the implants in the present study. Thus, the clinician should consider these techniques first if implant removal becomes necessary. Treatment planning for the post-removal site should be considered prior to implant removal. After removing a failed implant, the placement of an immediate replacement implant is often dependent on the amount and distribution of residual bone. Several authors have stated that following implant or tooth removal that guided bone regeneration (GBR) procedures are unnecessary for four-wall socket sites with no fenestrations or dehiscences and a gapdistance <2 mm between replacement implant surface and surrounding bone walls. Figure 1. Removal of a stripped screw, ruptured implant and external type implant with the versatile CEK instrument.8,9
However, if the implant socket contains fewer than three walls, use of GBR procedures as well as knowledge of the classification of the extraction socket type is helpful in treatment planning the augmentation of the socket defect prior to placement of a new implant.
tissue. 13,14 The bone healing response with piezo surgery also seems to be more favorable than that with burs. 15
10 However, when deep cuts in bone are necessary, the cutting speed of the piezo tips is decreased and this results in a rise in temperature. Therefore, cooling of the tip by intermittent cutting, the use of copious irrigation with cold saline and constant movement of the tip is
recommended.

Figure 1. Removal of a stripped screw, ruptured implant and external type implant with the versatile CEK instrument
In the anterior maxillary esthetic zone, an immobile failed implant should always be removed whenever possible by using a reverse torque technique in order to preserve soft and hard tissues.
Moreover, preservation of the bone during removal of the implant can help avoid or reduce the necessity of future augmentation procedures to allow placement of a new implant.
This is essential because the literature suggests that replacement implants have a decreased survival rate.
High-speed Burs
The use of high-speed burs under copious irrigation 11,12 is an efficient technique to remove a failed implant. The burs of choice are thin, tapered diamond burs. Channels should be cut on the mesial and distal aspects The following review of the implant removal techniques will vary from the least to most invasive in terms of collateral damage to surrounding soft tissue, bone and teeth.
Removal Instruments, Indications and Techniques: Counter-ratchet and Reverse Screw Techniques (CRT and RST)
These techniques are the least invasive in removing an implant without damaging surrounding structures. Cases amenable to removal with counter-torque ratchets depend on the implant connection (external hex/internal hex), patency of the internal or external connection, implant diameter, implant geometry, implant location (bone quality), and amount of osseointegration remaining.
The use of counter-torque wrenches should be considered the option of choice if the implant is able to be engaged and reversetorqued until mobile (Fig. 2).

Figure 2. Counter-ratchet technique (CRT)
RST is the second of the less invasive techniques, indicated in the removal of a fractured implant when the connection is damaged or in the removal of an external connection implant when the counter-torque ratchet cannot be engaged (Fig.3).

Figure 3. Reverse screw technique (RST)
Bone Removal Techniques (BRTs)
Piezo Tips
The use of piezo tips to remove bone surrounding an implant is less invasive than high-speed burs during cutting, because they prevent damage to the surrounding soft of the implant to avoid damaging buccal and lingual bone. However, air from the high-speed handpiece may
be forced into a surgical wound or a laceration in the mouth, causing an air embolism.
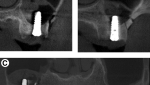
Trephine Burs
There are several sizes of trephines available correspond- 16 ing to various implant diameters. The smallest effective-size trephine should be selected to avoid collateral damage to the neighboring bone, teeth and/or implants (Fig. 4), and the internal diameter of the trephine should be slightly larger than the implant to avoid engaging the implant body. The preferred speed when using a trephine is 1,200 rpm to 1,500 rpm with copious irrigation. This technique is one of the most invasive options for implant removal. Fatigue fracture of the mandible after the use of a trephine bur has been reported, When using high-speed burs, the residual apical part of the implant should be approached carefully when in proximity to vital structures such as the sinus membrane, inferior alveolar nerve and mental foramen, in order to prevent damage to
these.

Figure 4. Bone removal technique (BRT) with a trephine
Moreover, pieces of the implant surface may enter the healing wound and should be removed by frequent saline irrigation as part of the procedure. Before using the burs, accurate radiographs to locate anatomical structures are recommended.
and osteomyelitis is another complication that may occur following explantation with a trephine bur if bone is overheated. 18 Thus, trephine burs are only indicated when absolutely necessary, and the retrieval procedure should be carefully planned and performed under copious irrigation withrefrigerator-cooled saline.
Again, intermittent cutting is recommended, moving the trephine in an apical then coronal direction. For those implants with expanded
platforms, the implant platform should be trimmed or resected in order to use the smallest diameter of trephine burs possible.
Often, only the coronal half of bone around the implant requires removal in order to loosen the implant, at which point elevators, forceps
and, where possible, torque drivers may be employed as part of a combination technique described below.
Combination Techniques
When an integrated implant cannot be removed with less invasive methods, piezo tips and/or high-speed diamond burs should be used to remove sufficient supporting bone around the coronal parts of the implant.
The countertorque ratchets or forceps should then be employed to remove the implant, to reduce the damage to the surrounding bone (Fig.5).

Figure 5. Combination technique, BRT + RST
Whenever burs are used, cuts should be made on the mesial and distal aspects of the implant.
Alternating between the counter-torque ratchet and the elevator and occasionally drilling with the tapered diamond burs or trephines can then be used in combination to remove the implant.
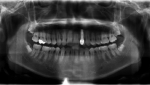
One of the subjects in this study was referred to the Ashman Department of Prosthodontic Dentistry at the NYUCD for removal of failed implants. The subject presented with 10 failing implants affected by peri-implantitis. Due to the different degrees of severity and bone loss
caused by peri-implantitis, 3 different techniques were required to remove these implants. Four of the mobile implants were removed by
forceps.
The other 6 implants were removed with RST and trephine burs (Fig.6-10).

Figure 6. A panoramic radiograph of all failed implants
This case was interesting, in that indications and limitations of the two less invasive techniques and BRT were all apparent within one
subject.

Figure 7. Before implant removal

Figure 8. Implant removal with BRT (left) and RST (right)

Figure 9. The extracted teeth and implants

Figure 10. The healed maxillary and mandibular ridges following implant removal
Limitations and Considerations of Less Invasive Techniques
The choice of implant removal technique should be based on the specific clinical factors such as patency of the internal or external connection, implant site, remaining amount of bone, anatomical conditions at the implant site, and bone quality. However, there are limitations and possible complications that should be considered in treatment planning implant removal.
Counter-ratchet Technique (CRT)
The CRT is a convenient and minimally invasive technique for implant removal. However, to utilize this technique, the connection component should be firm and solid. When used with external hexed implants, with limited height for the connection component,
CRT can easily destroy the connection. Therefore, RST should be considered to remove external connection implants. When used with internal connections, at the connection level, the connection should not demonstrate any sign of a crack, rupture or fracture that can result in further fracture of the implant when the CRT is applied (Fig. 11). In such circumstances, RST can be the indication for the implant removal.

Figure 11. Implant fracture at the connection level
Reverse Screw Technique (RST)
The RST was used to remove more than 30% of the implants in the present study. RST devices may require 200 Ncm to 400 Ncm to remove an implant, depending on the type of RST used. The taper and diameter of the device also affects the torque that can be generated. The greatest torque is usually obtained when the device reaches the apex of the screw hole (Fig. 12).

Figure 12. Proper binding between the RST device and implants
In the 41 cases in which the RST was used, there was 1 fracture of the device at the connection level (CEK generates up to 250 Ncm according to the EBI). In another case, the RST device was able to break the osseointegration (Fig.13).

Figure 13. RST failed due to the circular thread design of the implant
However, due to the circular thread design of the implant, it remained rotating but was not able to be removed.
A trephine bur was ultimately needed to remove this implant. Therefore, use of RST is ontraindicated for non-screw-type implants that have
undercuts (i.e., Bicon or Paragon micro-vent implants).
Other Less Invasive Techniques in the Current Literature
A recent case report by Cunliffe et al described the removal of a dental implant using
electrosurgery.
An ultrahigh-frequency monopolar electrosurgery unit was applied to the internal surface of the neck of the implant to cause thermonecrosis at the bone-to-implant interface.
After one week, with the aid of the CRT technique, the implant was removed.
This report demonstrated that heat treatment of failed implants can be used as a minimally invasive technique to remove an implant.
However, reliable methods of regulating the heat to implants, the human threshold and possible complications including bone necrosis should be further studied prior to recommending this technique.
Moreover, the extent of bone necrosis and repair may complicate placement of a new implant in the same site.
Other authors (Pattison et al) have suggested the interposition of a foil from a suture pack between the RST device and the implant connection.This can increase the stability of the connection enough to allow for removal.
However, this technique also requires more research.
Conclusion
Treatment planning of the post-removal site should be performed prior to implant removal. The use of less invasive implant removal techniques can provide more treatment options and better treatment outcomes. The results of the present study demonstrated a 60% retrieval rate using less invasive techniques. Thus, the clinician should consider these less invasive methods first if implant removal becomes
necessary. More research on this subject is needed to evaluate the effectiveness and applicability of these techniques and verify the findings in the present report.