Mini-Lateral Windows for Minimally Invasive Maxillary Sinus Augmentation: Case Series of a New Technique
Leon Pariente, DDS, Karim Dada, DDS,* and Marwan Daas, DDS, MS, PhD†
The sinus augmentation proce- dure using the lateral window technique is a well-documented method for increasing bone volume in the posterior atrophic maxilla.1–4 The goal of this procedure was to provide adequate bone volume for implant placement.
The success of a sinus augmenta- tion procedure can be measured by the survival rate of implants placed in that bone under functional load and by the quantity and quality of vital bone formed in the pneumatized sinus after graft maturation.4
Implant survival rates in grafted
sinuses have been reported to be influ- enced by the bone graft material, the presence or absence of a membrane over the window, and the implant surface characteristics. The implant placement timing (simultaneous vs delayed) and the residual crestal bone height are parameters that have also been exam- ined.1,2,4 Evidence-based literature re- views reported an average implant survival rate of 91.8% with a range of
61.7% to 100% for the lateral window sinus augmentation.1,2 Simultaneous and delayed implant placement showed similar survival rates of 92.17% and
92.93%, respectively. In the same study,
*Dentist, Private Practice, Paris, France.
†Associate Professor, Department of Prosthodontics and
Implant Dentistry, University Paris V, Paris, France.
Reprint requests and correspondence to: Leon Pariente, DDS, 62 Boulevard de la tour maubourg, 75007 Paris, France, Phone: +33669499790, E-mail: leonpariente@ gmail.com
ISSN 1056-6163/14/02304-001
Implant Dentistry
Volume 23 Number 4
Copyright © 2014 by Lippincott Williams & Wilkins
DOI: 10.1097/ID.0000000000000119
Objectives: The purpose of this article was to introduce a new tech- nique for minimally invasive lateral window sinus augmentation, developed to maximize the amount of residual lateral wall after the procedure.
Materials and Methods: Four- teen consecutive patients requiring maxillary sinus augmentation by a lat- eral approach and delayed implant placement were treated using stan- dardized mini-lateral windows. Before the procedure, the remaining height of alveolar bone was determined;
6 months after the procedure, the augmented height and augmented width were measured. The extent of the antrostomy was calculated using a gauge and compared with a conven- tional window size.
Results: A total of 15 maxillary sinus augmentation procedures
the survival rate for implants having smooth and rough surfaces was 85.64% and 95.98%, respectively.2
Vital bone formation in the pneu-matized sinus can be affected by several factors. These factors include: type of graft or graft replacement material used, use of a barrier membrane over the lateral window, healing time, and sinus anatomy.5–7
Autogenous bone (AB) has long
been considered the gold standard as a graft material because of its osteoin- ductive and osteoconductive properties.2
However, many allografts, xenografts, were performed in 14 patients using this technique. Every patient received the planned implant treatment 6 months after the sinus augmentation procedure. The average residual bone height was 2.1 6 1.1 mm, the average augmented height was 13.4 6 3.4 mm, and the average aug- mented width was 19.0 6 5.5 mm. The average total area of the antros- tomy was calculated to be 59.2 6 12.8 mm2.
Conclusions: The results of this case series study suggest that this technique allows for the achievement
of a similar result as with conven-tional size windows, but with a sig- nificantly smaller total window area.
(Implant Dent 2014;23:1–7)
Key Words: lateral window dimen- sion, membrane elevation, second
window
and alloplastic graft materials have also been used, alone or in combination with AB, for the sinus augmentation proce- dure.5,8–11 Hallman reported vital bone formation with different grafting mate- rials including AB, bovine hydroxyap- atite (BH), or a 20:80 mixture of AB and BH after a 6 to 9 months healing period. The vital bone content was 37.7%, 39%, and 41% for AB, mixture of 20% AB and 80% BH, and 100% BH, respectively. This histomorpho- metric analysis showed no statistically significant difference in vital bone for- mation regardless of the graft material
used.12 The literature shows a wide range of results using different grafting materials.6,10,11,13–21
Use of barrier membranes has been shown to increase vital bone formation. Tarnow et al6 performed 12 bilateral sinus grafts and reported 11.9% vital bone for the side without the membrane and 25.5% for the side with the mem- brane. Avera reported similar clinical and histological results using an absorb- able membrane made of polylactic acid compared with a nonabsorbable mem- brane of expanded polytetrafluoroethy- lene in lateral wall sinus augmentation procedures.13
Wallace et al7 reported that time of healing was a positive factor in the amount of vital bone formation. In that study, the xenograft material was com- pletely resorbed and replaced with vital
bone during 12 to 20 months healing period. Valentini confirmed that anor- ganic bovine bone allograft (ABBA) has good osteoconductive properties. Six months after sinus augmentation with ABBA, 57 implants were placed into the augmented sinuses. New bone formation was confirmed and calculated in biopsies of 3 patients, which showed an average of 21.08% new bone after 6 months and
27.55% after 12 months. Average residual ABBA was reported as 39.17% after 6 months and 27.01% after 12 months. After a mean loading period of 4.0 6 0.5 years, 56 implants remained in place.9
However, other histologic studies reported different results for time of xeno- graft resorption.6,10,11,13–21
Recently, a new factor has been introduced by Avila-Ortiz et al22: the dimension of the lateral window. They were the first to report a negative correlation between the average window dimension and the percentage of vital bone with a high statistical significance when grafting with an allograft.22 They also observed a positive correlation between the size of the window and the percentage of remaining particles of allograft after 6 months of healing. Although allograft particles were solely used in this study, these results suggest that the preparation of large lateral win dows for maxillary sinus augmentation negatively influences the rate of vital bone formation. The technique to create the lateral window and access to the
Schneiderian membrane seems to be a crucial factor.
After Tatum,23 Boyne and James24 introduced the lateral window for sinus augmentation procedure, in which var- ious instruments have been used for the creation of the lateral window and the elevation of the Schneiderian mem- brane. The window was originally prepared with the use of the slow-speed surgical handpiece.23,24 Later, other clinicians began to use the high-speed handpiece for the window preparation. Although these techniques were accept- able, they were not without risks. The intraoperative complications of mem- brane perforation and bleeding were ad- dressed by a new technique, designed to minimize the complications of sinus augmentation surgery. The Piezo-elec- tric surgery concept (Piezosurgery) was introduced by Vercellotti25 as a method to decrease the incidence of perforation of the Schneiderian membrane, which had been one of the most common com- plications of the lateral window sinus augmentation procedure.26 A perceived disadvantage of the use of Piezosurgery is the additional time that may be nec- essary for the preparation of the win- dow in the lateral wall.
The dimensions of the lateral window are commonly determined by the amount of augmentation required, which is directly related to the number of missing posterior teeth that need to be replaced. Whereas antrostomy size of 20 mm mesiodistally and 15 mm apico-coronally (surface area of 300 mm2) are sufficient to guarantee easy surgical access.27 For experienced op- erators, smaller windows are described in the literature; 14 mm height and 6 mm width (surface area of 84 mm2) seems to be an admitted average size for conventional windows.25 Despite being one of the key points of the pro- cedure, there is a lack of literature on the surface area of the window. Avila- Ortiz et al22 reported an average window surface area of 69.71 mm2, and Barone et al28 described window surface area of 137 mm2.
The purpose of this article was to introduce a new technique for mini- mally invasive lateral window sinus augmentation and to report 15 cases of sinus augmentation made using this technique preliminary to a prospective clinical study.
MATERIALS AND METHODS
This case series consisted of 15 con- secutive maxillary sinus augmentations using the lateral window approach and delayed implant placement. All patients received maxillary sinus augmentation surgery to allow the placement of endo- sseous implants between September
2012 and March 2013 at 62LTM pri- vate practice (Paris, France).
Preoperative intraoral examination was performed along with cone beam computed tomography (CBCT) in each
case. Patients were provided with treatment plans, including all relevant options. Written consents for the procedures were obtained. Computed top- ographies were performed 6 months after the sinus elevation to plan for implant placement.
Surgical Procedure
Preoperative Medications. Antibiotic treatment (Amoxicillin 500 mg, 4 per day for 7 days) was started 24 hours before the surgery. Patients allergic to Penicillins were requested to take Clindamycin 300 mg per day for 7 days. On the day of surgery, the patients received a dose of Attarax (1 mg/kg)
1 hour before the surgery as sedative premedication.
Surgery. Local anesthesia was per- formed with local infiltration and greater palatine nerve block anesthesia using 2% of lidocaine with 1/100,000 epinephrine (3M ESPE).
A midcrest incision was made, and the distal limit for this incision was established 5 mm distally to the position of the planned most distal implant. The incision was extended mesially intra- sulcularly to the first bicuspid when it was present. Two vertical incisions were prepared from the mesial and distal end of the horizontal incision, extending up to 5 mm apically beyond the mucogingival junction. A full- thickness flap was then elevated allow- ing a complete vision of the lateral wall of the sinus (Fig. 1). A sinus kit with microsurgical instruments, the EBI Sinus Kit (EBI North America, New York, NY, USA) was used to determine the size of the windows and proceed through the membrane elevation. The SCC4 instrument, which presents a probe type side and an ovate shape side, was used on its probe type side to locate the most apical portion of the window corresponding to the apical part of the implant planned in the most mesial position. The ovate shape of the SCC4 instrument was used to draw the windows in the lateral wall of the sinus.

fig. 1. Buccal view of the lateral wall of the maxillary sinus after flap elevation.
It has an elliptic shape of 5 mm height (a) and 8 mm length (b): its total area was calculated to be 31.4 mm2. Because it appeared that drawing the window with the gauge did not prevent from clinical variation after the window was completed, the maximal height (a) and maximal width (b) of the ellipsoidal window were measured during the surgery using a periodontal probe on the mesial window (mesial Window Clinical Dimensions) and on the distal
window when present (distal Window Clinical Dimensions). In all cases, the size of the first window was made using this instrument as a gauge. The window was prepared using a round diamond coated sinus lift tip on the Piezotome (SL2; Satelec-Acteon, Bordeaux, France). The bone was del- icately removed on the entire area of the planned window until the mem- brane was visible and could be ele- vated using a flat-ended noncutting tip on the Piezotome (SL3; Satelec) (Fig. 2), the SCC1 (Fig. 3) to reach the anterior limit, the SCC2 instru- ments (Fig. 4) to reach the posterior limit, and the SCC3 to reach the medial wall (Fig. 5). In cases where a single implant was planned, this was the only window to be prepared. In cases where multiple implants were planned, the second window was pre- pared the same way distally at the api- cal portion of the planned most distal implant (Fig. 6). The size of this win- dow was first prepared half the size of the gauge and was extended to the full size of the gauge when necessary, that is, when a tear in the membrane was detected, to manage excessive bleed- ing, to help to elevate the Schneiderian membrane or allow better visibility or access.

fig. 2. Buccal view of the beginning of the elevation of the Schneiderian membrane. The instrument used is a flat-ended noncutting tip (SL3; Satelec) on the piezotome.

fig. 3. The Schneiderian membrane is ele- vated anteriorly using the SCC1 instrument (EBI) through the first window.

fig. 4. The Schneiderian membrane is ele- vated posteriorly using the SCC2 instrument (EBI) through the first window.
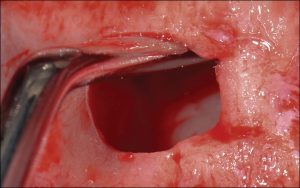
fig. 5. The medial wall of the sinus is reached using the SCC3 instrument (EBI).

fig. 6. The second window, half the size of the first one is created distally to the first one with the round diamond coated sinus lift tip (SL2; Satelec).

fig. 7. The SCC4 instrument (EBI) used as a gauge to create the window is also used to pack the xenograft into the maxillary sinus.
In each case, even in the absence of visible membrane tear, a resorbable collagen membrane (Bio-Gide, Geistlich, Paris, France) was placed over the mem- brane before placing the bone graft into the sinus. All augmentations were accomplished with xenograft (Bio-Oss; Geistlich) (Figs. 7 and 8). All lateral win- dows were covered with a resorbable col- lagen membrane (Bio-Gide; Geistlich) (Fig. 9). The full-thickness flaps were repositioned and sutured into place with 5-0 Vicryl (Ethicon) horizontal mat- tress and interrupted sutures. After each surgery, any membrane perforation or abnormal perioperative bleeding were reported in the patient’s chart.

fig. 8. Buccal view after placing the xeno- graft (Bio-Oss; Geistlich) into the sinus.
Postoperative Care. All patients received amoxicillin 1 g 2 times per day for 7 days subsequent to the surgery. Ibuprofen 400 mg 4 times per day for 7 days was prescribed for pain management. Oral hygiene instructions were given along with prescription for
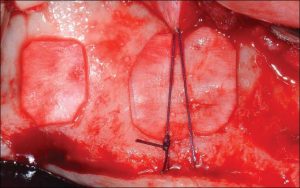
fig. 9. Two collagen membrane (Bio-Gide; Geistlich) are trimmed and placed over the windows, horizontal mattress sutures are used for stabilization.
chlorhexidine mouthwash twice daily for 2 weeks. Patients were seen for control visit 1, 2, 6, and 12 weeks after surgery. A cone beam CT scan was performed after 6 months of healing to plan for implant placement.
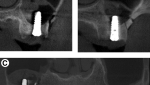
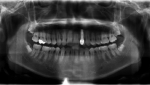
CBCT Analysis. The CBCT were col- lected, anonymized and reviewed by 2 calibrated blinded examiners, radiolog- ists from the University of Paris V. They were asked to measure the re- maining alveolar bone (RAB) height on the preoperative CBCT, the maximal augmented height (MAH), the maximal augmented width (MAW) on the 6 months postoperative CBCT. Maximal height and width were averaged and expressed as their mean value between the average of the 2 sets of measure- ments (Fig. 10).
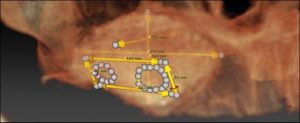
Fig. 10. Three-dimensional view of the CBCT 6 months after the sinus surgery. The 2 windows and conventional windows are drawn on the lateral wall.
Fourteen patients, 8 women and 6 men, with a mean age of 55.3 6 10.8 years (range, 35–72 years) participated in the study. As part of the usual pro- tocol in the office, after the CBCT anal- ysis, 3 patients were referred for otorhinolaryngology medical consulta- tion because of maxillary sinus abnor- malities (eg, thickening of the sinus membrane or mucous retention cysts). All were cleared to proceed with the surgical intervention. One patient underwent a bilateral maxillary sinus augmentation, a total of 15 sinus eleva- tion procedures were therefore per- formed. In each procedure, the total volume of xenograft used ranged from
2 to 5 cm3. The clinical and radio- graphic measurements are reported in Table 1. The mean RAB height was
2.1 6 1.1 mm. The MAH obtained was 13.4 6 3.4 mm. The MAW (in mesiodistal direction) obtained was 19.0 6 5.5 mm. The Clinical Window Area (CWA) was calculated using this formula: CWA ¼ 1/4 3 p 3 a 3 b. The mean value for CWA was 59.2 6
12.8 mm2. It can be compared with the Gauge Calculated Window Area, which would be the area obtained from a per- fect drawing of the gauge on the lateral wall: 52.3 6 11.4 mm2.
The surgical parameters are reported in Table 2. The incidence of membrane perforation was 13.3%. In the 2 cases that perforations were visi- ble, there were no larger than 3 mm (as measured with a periodontal probe) and were sealed intraoperatively
|
Case No. |
RAB (mm) |
MAH (mm) |
MAW (mm) |
mWCD (a/b) (mm) | dWCD (a/b) (mm) |
CWA (mm2) |
GCWA (mm2) |
Ratio WW/AW (%) |
| 1 | 1.5 | 11.2 | 14.6 | 6/8.5 | 6/4 | 58.9 | 47.1 | 85.6 |
| 2 | 4.6 | 16.6 | 18.1 | 5.5/8.5 | 5.5/8 | 71.3 | 62.8 | 91.2 |
| 3 | 2.8 | 9.7 | 16.6 | 5/8 | 5.5/4 | 48.7 | 47.1 | 72.3 |
| 4 | 1.3 | 13.1 | 22.0 | 5.5/8 | 5.5/8.5 | 71.3 | 62.8 | 75.0 |
| 5 | 1.0 | 13.0 | 21.2 | 6/8 | 5.5/4 | 55.0 | 47.1 | 56.6 |
| 6 | 2.0 | 13.6 | 18.8 | 5.5/8.5 | 5/4 | 52.4 | 47.1 | 66.5 |
| 7 | 2.5 | 10.7 | 13.6 | 5.5/8.5 | 5/4 | 52.4 | 47.1 | 91.9 |
| 8 | 1.3 | 18.6 | 20.7 | 5.5/8 | 6/8 | 72.3 | 62.8 | 77.3 |
| 9 | 3.2 | 16.0 | 20.9 | 6/8 | 5.5/8 | 74.4 | 62.8 | 76.6 |
| 10 | 2.3 | 16.4 | 27 | 6/8 | 5/4 | 54.7 | 62.8 | 44.4 |
| 11 | 0.4 | 11.8 | 26.2 | 5/8 | 5.5/8 | 68.1 | 62.8 | 61.1 |
| 12 | 1.1 | 19 | 28.0 | 5.5/9 | 6/8 | 76.6 | 62.8 | 60.7 |
| 13 | 2.4 | 14 | 16 | 6/9 | 5/4 | 58.1 | 47.1 | 81.3 |
| 14 | 3.2 | 7.8 | 10.9 | 5.5/8 | NA | 36.7 | 31.4 | 73.4 |
| 15 | 1.6 | 8.9 | 10.2 | 6/8 | NA | 37.7 | 31.4 | 78.4 |
| Mean 6 SD | 2.1 6 1.1 | 13.4 6 3.4 | 19.0 6 5.5 | 5.6 6 0.4/ | 5.4 6 0.4/ | 59.2 6 12.8 | 52.3 6 11.4 | 72.8 6 13.1 |
| 8.3 6 0.4 | 5.9 6 2.1 |
series was to evaluate the potential benefits and limitations of using these mini-invasive lateral sinus wintions where the residual alveolar bone
height is limited, the quality of the future interface bone-implant relies mainly on the healing and maturation of the graft. It requires the use of the full potential of osteogenic capacity of the maxillary sinus walls.
The first issue of this type of study was to standardize the size of the lateral windows for each case for proper evaluation. To attempt to solve this matter, the ovate side of the SCC4 instrument of the sinus kit (EBI) was used as a gauge. This instrument was chosen from among the other instru- ments because each of the other instru- ments of this mini-invasive sinus kit
using a resorbable collagen membrane (Bioguide; Geistlich). There was no report of preoperative or postoperative bleeding.
The patients were regularly fol- lowed for the 6-month healing period. No patient suffered from sinus infection or abnormal postoperative bleeding. In all cases, the bone augmentation achieved after sinus augmentation allowed implant placement as planned in the initial treatment plan. The dura- tion of the surgery did not exceed 40 minutes in each case. This is in the same timeframe as with conventional windows in our daily practice.
DISCUSSION
The use of single or multiple mini- invasive lateral sinus windows has, to the best of our knowledge, never been discussed in the literature. However, in cases where septa are present, the use of multiple lateral windows has been described. The purpose of this case
could be passed and used through a window of this size and shape. It appeared that the obtained windows were not the exact size of the gauge, and that there were small irregularities (#1 mm) in height or length due to the free-hand surgical technique used.
Therefore, measurement of the maxi- mal height (a) and width (b) of the ellip- soidal shaped windows were made using a periodontal probe. The stan- dardization of the windows was already described as an issue by Avila.8 The developments of bone reamers to create the lateral windows seem promising and should be evaluated as a mean of achieving perfect standardization in additional studies.
The clinical indication for sinus elevation varies from 1 to 4 implants. Those variations in indication have an influence on the procedure. The amount of bone augmentation is different, and the need for distal extension of the augmena positive influence in cases where there is lack of osteogenic potential: when using xenograft particles only for sinus grafting and when the residual alveolar bone height is limited.
In this case series study, the mean ratio between the total window length and the total augmented width was calculated to be 72.8 6 13.1%. This ratio averages 100% in a conventional approach. The lower values were found a similar result with a window area that is smaller than conventional techniques. It would be of prime interest to investigate, in a prospective human study, the influ- ence of this technique on maturation of the bone, on consolidation of the graft and on the vital bone formation after maxillary sinus augmentation.
DISCLOSURE
etation varies also significantly. As a result, in cases where the maximal augmented fi The authors claim to have no it appeared that in cases where a single implant placement was planned only 1 window of the size of the gauge (31.4 mm2) was necessary. Attempts were made to achieve the procedure with only 1 half-size window. However, in the 2 cases reported in this case series study, it was rendered necessary to enlarge the windows to a full gauge size to achieve satisfactory results.
When multiple implants were planned, the second window was used. The size of the second window could be, first, limited to only half the size of the gauge. The second window could then be extended to a full-size window, to reach the limits of the needed aug- mentation, if there were any difficulties in the membrane elevation or in cases of surgical complications such as tear of the membrane or bleeding.
The amount of lateral bone that can be preserved compared with conven- tional size windows may be clinically relevant in some situations where high osteogenic capacities are necessary. The sinus augmentation relies on the same principles as other bone regeneration procedure: the osteogenic potential of the walls surrounding the graft is crucial. The immediate benefice of maintaining
this band of bone intact is that it helps to contain the biomaterial. It has also been reported that the lateral wall of the sinus has a high osteogenic capacity.29 Pre- serving a large area of lateral bone could therefore enhance the healing in improv- ing the consolidation and maturation of the graft as well as the vital bone forma- tion. In cases of delayed implant place- ment protocol, the mechanical stability and the osseointegration of the implant rely solely on the properties of the regen- erated tissue.
Preserving as much as possible the lateral wall of the sinus could have width were the highest, when the oste- ogenic potential of the lateral wall of the sinus is the most necessitated.
The incidence of membrane perfo- ration using this technique was shown to be in the same range as the perfora- tion rates of conventional techniques (13.3% vs 23%).28 All perforations occurred during membrane elevation.
It was of prime importance to demon- strate that preparing the second window does not increase the perforation rate. Likewise, it was not observed that the second window, or smaller window, affect the preoperative or postoperative bleeding as well as the capacity to obtain the desired bone augmentation for proper implant placement. Under no circumstances in any of the cases, it was necessary to increase the size of the windows to a conventional window size. When a repair of the Schneiderian membrane was rendered necessary, a collagen membrane (Bio-Gide; Geist- lich) could easily be folded and placed to patch up the Schneiderian membrane by using microsurgical forceps through both windows access.
Furthermore, the small sizes of the windows and the flexibility in the planning of their positions allowed avoiding the maxillary artery when it was visible on the CBCT scan. It is important to note that this technique did not require additional time for the surgery as compared with the conven- tional technique and, therefore, can be used routinely in a daily practice.